The Case for Veterinary Nurse Practitioners
We covered what a veterinary nurse practitioner’s role may include, as well as some of the most commonly heard pros and cons of adding this new role to the profession.
This week, we’re covering some additional pros and cons for discussion, as well as practical considerations for when and how this change may occur in vet med.
Read on to learn more…
Veterinary Technician Utilization and Career Growth
It’s no secret that veterinary technicians are often underutilized and that their pay is often not up to the standards of their professional education and the crucial role that they play at a veterinary practice.
Many technicians note there is a “ceiling” for them in clinical practice—in terms of reaching new levels of professional satisfaction and an income that truly reflects their knowledge and hard work.
As such, many vet techs leave the clinical side of the work they love in order to pursue management, teaching, or even an entirely new start in human medicine or another field.
Many argue that a veterinary nurse practitioner option would help more techs stay in the field and be appropriately compensated while continuing to grow professionally.
On the other hand, many have pointed out that it may make more sense to fully utilize vet techs (and pay them a higher compensation) prior to creating a new role.
In other words, if we don’t fix the current problems vet techs are facing, would those issues just be perpetuated in a new role?
Less of a Role for Veterinary Technicians
Those who don’t support the veterinary nurse practitioner movement point out that once this new role is created, there may be less of a need for traditional vet techs.
These wonderful staff members may begin to feel underutilized, underappreciated, and underpaid next to their new nurse practitioner coworkers—since nurse practitioners would still be able to perform all the tasks a vet tech could.
Veterinarians Fully Utilizing Their Education versus Daily Routine Appointments
While a nurse practitioner role may help vet techs see their full professional potential, some argue it will carry the same benefit for veterinarians.
If a vet’s time is freed up from repetitive daily wellness and minor issues appointments, they may be freer to pursue their own professional interests, such as dentistry, surgery, acupuncture, complicated internal medicine cases, or anything else they enjoy.
Of course, many vets do enjoy daily interactions with clients for more routine appointments, so this may depend on personal preference.
And some worry that the loss of those daily, routine interactions could hurt their relationships with clients in the long-term—that they would only see clients when their pet is seriously ill, without a prior relationship.
Preventing Burnout Within the Profession
Many veterinarians and veterinary professionals have suffered from burnout and mental health concerns related to their careers.
Some state that a veterinary nurse practitioner role can help the profession as a whole in this regard—by taking some of the extraordinary workloads off of veterinarians and delivering better workflow to the whole practice.
Also, allowing skilled veterinary professionals to receive fair compensation and derive more professional satisfaction could help with job satisfaction for the whole team, not just vets.
Consumer Expectations and Preferences
It’s been pointed out that veterinary medicine, in general, is slow to update to new technology and consumer preferences.
Some argue that veterinary nurse practitioners may be expected by pet owners in the near future, since that’s what people are used to for their own health care.
While many veterinarians and practice owners expect clients to stick to the practice’s way of doing things, history in many other industries has shown us that customers eventually do turn elsewhere when businesses fail to adapt to the times.
Distribution of Veterinary Services
Whether there is a national surplus or shortage of veterinarians, some parts of the country have faced a vet shortage in either climate—especially rural areas.
For this reason, some rural practitioners have voiced their support of the veterinary nurse practitioner, as it may be a way to distribute some of their caseloads even when they can’t find a DVM to hire.
Others argue that while nurse practitioners would be more affordable than a DVM, they would still be too expensive for some rural practices—and that these practices would be hurt in the long run because there would be fewer traditional vet techs overall for them to hire.
Liability
One serious concern to answer is who is legally responsible if a medical error occurs while a patient is under the care of a veterinary nurse practitioner?
If the veterinarian is liable, as is the case when an error occurs by a vet tech, this may make veterinarians reluctant to delegate.
When and How Could the Role of Veterinary Nurse Practitioner Be Created?
While there is much discussion about this topic right now, it could take quite a while for any serious changes to be made toward the creation of this new role.
Some of the roadblocks include the need for major changes to education and credentialing.
Currently, many vet techs have an associate degree—which is much shorter than the length of time required to become a veterinarian. Supporters of the nurse practitioner role envision the degree being the equivalent of a master’s degree, so the education would be much more extensive.
Additional considerations include accreditation of any educational programs, as well as standardization for credentialing, continuing education, etc.
Also, there’s the matter of what the state laws allow vet techs to do at a veterinary practice. These laws would have to be changed, and that could take years and be very expensive.
What’s Next?
It’s been suggested that more data is needed to know if the nurse practitioner is really sustainable for the long-term (and not just a short-term need during the pandemic), and that it may take many years for this new role to be created.
On the other hand, at least one university is in the process of creating a master’s degree targeted to veterinary technicians.
There is certainly some appeal to the collaborative environment envisioned by supporters, with a healthier workload distribution to all employees while allowing the practice to provide high-quality care to more pets and bring in more revenue.
But while there may be benefits, it’s certainly necessary to continue discussing any potential downsides so that there is a realistic idea of how this new potential role could affect the profession as a whole.
Additional great sources of information include a recent podcast from Dr. Andy Roark
and an article from VIN News Service (https://news.vin.com/default.aspx?pid=210&Id=10484775 ).
Written by: Dr. Tammy Powell, DVM
Does the Profession Need a Veterinary Nurse Practitioner?
A hotly debated topic in veterinary medicine right now is whether there is a need for a midlevel practitioner—a position comparable to a nurse practitioner or physician’s assistant on the human side of medicine.
So, what are the arguments for and against this potential new veterinary career track? And what would be required for the role of veterinary nurse practitioner to be created?
This is what will discuss today, in the first part of a two-part series on midlevel practitioners in veterinary medicine…
What Is a Veterinary Nurse Practitioner?
A midlevel practitioner is someone whose scope of practice would be beyond that of a veterinary technician or nurse, but less than that of a veterinarian.
This idea has been floating around for at least a decade, if not longer. But the recent veterinarian and vet staff shortage during the pandemic may have spurred to the forefront of many vet professionals’ minds.
Right now, veterinary technicians are able to perform many of the tasks necessary for patient care. The exception is any part of the scope of practice that is limited to vets—diagnosing, prognosing, prescribing, and performing surgeries.
Creating a veterinary nurse practitioner would mean allowing these vet professionals to take on some of these roles that are currently restricted to veterinarians.
Examples may include taking on wellness visits, diagnosing and prescribing treatment for minor ailments (ear infections, etc.), refilling chronic medications after checking bloodwork or performing minor surgeries such as uncomplicated dental extractions.
Of course, many tasks—including most surgeries and management of more in-depth medical cases—would continue to be reserved for licensed DVMs…
The goal of this new role would be to take some of the routine daily tasks off the veterinarian’s hands, to free up the veterinarian and allow the practice to provide care to more patients.
What Are the Arguments For and Against Creating Veterinary Nurse Practitioners?
There are strong cases being made both for and against this new position within veterinary medicine. Here are some of the key points of the debate…
Access to Care
Right now—as demand for veterinary care increased during the pandemic, while a shortage in vets and vet team members has left many practices struggling to keep up with that demand—many pet owners report challenges in receiving care for their pets.
Clients are having difficulty scheduling appointments, often having to wait weeks to months for a wellness visit. And some practices have limited how many new clients they can see.
Proponents of the veterinary nurse practitioner envision the role freeing up time for the vet, so that the practice can see more patients and clients.
On the other hand, some state that a decision that could permanently affect the future of the profession shouldn’t be made because of circumstances that could be short-term.
In other words, is the increased demand for pet care during the pandemic going to stick around? Is it enough to fuel and support the new role of the veterinary nurse practitioners in the long term?
Availability of Jobs for Veterinarians
Right now, there is a veterinarian shortage. But not so many years ago, many complained of a surplus, which made veterinarians’ jobs harder to find with less competitive salaries.
Detractors of the veterinary nurse practitioner movement worry that in another few years, we could again be facing a surplus of vets. After all, ups and downs are natural in any industry.
Should that occur at any point in the future, there is a serious concern that veterinarians could be out of work because practices (especially corporate practices) may prefer to hire lower-salary nurse practitioners rather than DVMs.
Since nurse practitioners in human medicine have the right to open their own practice, there is also a potential concern of competition for veterinarians who are practice owners.
Cost of Care
Even before staffing shortages occurred, the cost of care has been another hotly debated topic in veterinary medicine for many years. This is another important facet of access to care since many pet owners are unable to afford quality veterinary care.
Some state that by providing a midlevel practitioner, a veterinary practice can expand its reach to more clients by offering affordable services (since a veterinary nurse practitioner would be paid less than a veterinarian), especially for wellness and minor ailments.
Supporters argue it would be the best of both worlds. In addition to the ability to offer affordable services, the new system would also increase the practice’s bottom line and provide fair compensation to all employees (since having a nurse practitioner would allow a practice to see a lot more patients per day and thus bring in more revenue).
Also, the availability of nurse practitioners may decrease the need to hire relief vets for too many shifts, decreasing the practice’s overall operating costs. Of course, for relief vets, this would be a disadvantage.
Stay Tuned for More…
To cover this topic more in-depth, we’ll address more pros, cons, and considerations in next week’s article.
In the meantime, hopefully, this has provided some food for thought.
Whether the profession moves forward with creating a nurse practitioner role or not, the issue has opened discussions on many important topics currently facing the field of veterinary medicine. And those discussions are important to always improve, adapt, and to find solutions to keep the profession healthy and sustainable.
Written by: Dr. Tammy Powell, DVM
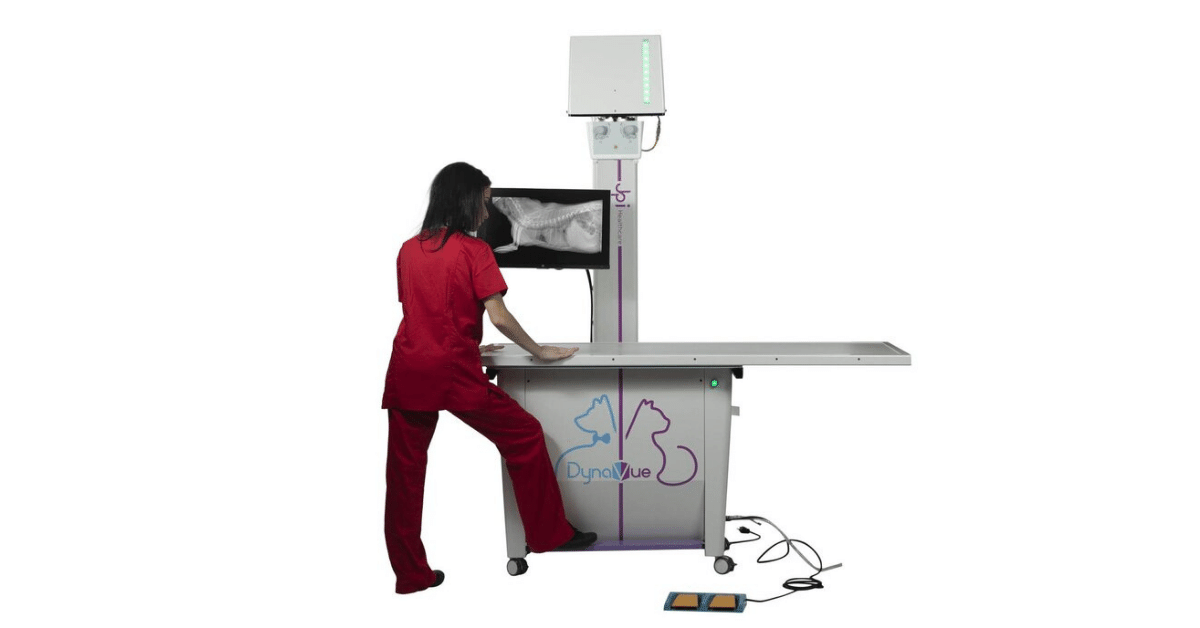
Veterinary Digital DR X-Ray JPI Directvet System
Veterinary Digital DR X-Ray System Package Deal
Regardless of healthcare professionals' skills and experience, the quality of medical care patients receive will only be as good as the equipment used. This applies not only to human beings and their doctors but to animals and veterinary healthcare practitioners. NewVetEquipment is the proud supplier of high-quality veterinary equipment and is pleased to offer the DirectVet Plus full Veterinary Digital X-Ray System.
Here's a closer look at what this system has to offer
DirectVet Plus X-Ray Table
Veterinarians have to handle pets and animals of all sizes, which means that the x-ray table they use needs to withstand the weight of larger animals. This 32x54-inch system can support more than 300 pounds of weight at a time, and the generator arm is designed to move back and forth over the subject. This makes the system capable of handling the x-ray needs of animals as large as ponies with relative ease.
CubeX 28 X-Ray Generator
CubeX is well-known and respected for its high-frequency, portable generators for veterinary and medical use. These x-ray generators are lightweight and compact. Veterinarians will be pleased with the CubeX 28 due to its user-friendly digital displays, simple design, and soft-touch controls. It comes with two-stage, dynamic auto-line compensation, dual integrated laser pointer, and an easy-to-use inverted control panel that makes it compatible for use with a table.
CareRay Cesium Flat Panel Detector
CareRay Digital Medical Systems is an industry leader in developing, researching, and manufacturing x-ray flat-panel detectors. This system comes with the 17x17-inch cesium flat panel detector that is packed with exceptional performance features, including:
High-definition filming: The high levels of detail these panels can produce make it possible for veterinarians and radiologists to diagnose tuberculosis, inflammation, tumors, and more. Experts will observe and make judgments regarding the biliary tract, abdomen, and urinary tract. These panels also facilitate skeletal viewing, muscular system observations, foreign body identification, and trauma diagnoses.
Image and Video Playback functionality: It comes with a playback function that allows you to save and review videos that highlight the motility and morphology of the organs in the gastrointestinal tract.
Visual contrast functionality: Barium-based imaging is often necessary for the x-raying and observation of the esophagus, angiographies, enemas, sinus fistulas, and other circumstances where observations need to be made compared to surrounding tissues.
Large-format perspective functionality: Veterinarians will be able to get a clear view of the pulsation of the heart and respiratory movement of the subject's lungs. This is made possible by the wide format of the flat panel's 17x17-inch layout. These clear and comprehensive radiographic images make the need for multiple imaging and repositioning unnecessary.
Easy integration: These flat panel x-ray detectors are easy to configure and integrate with whatever system you're using. This broad system compatibility will make the operator's or technician's life much easier.
All CareRay Digital flat panels are fully FDA, CFDA, CE, and ISO13485 certified and are widely used in the veterinary, medical, security, and industrial fields in various capacities. They are highly durable pieces of equipment made out of aluminum alloy and carbon fiber housing.
ExamVue PAC Software
The proper software has to be put in place to support the function of this system in an office setting. ExamVue has developed its simple, fast, and user-friendly software, with a very convenient diagnostic function. ExamVue PAC is server-based, and it comes with a series of advanced specialty tools, including line profiles, freehand, rectangle, polygon, and histogram. Image annotation is also made possible via user text, length, cobb angle, angle, and R/L mark.
Smaller practices and more extensive operations are accommodated by the system, with the capability of supporting up to 10 separate viewers. It has unique features and capabilities, including image stitching, importation, comparisons, processing, storage, and communication. It will work well with any DICOM DIR or Q/R compatible devices.
Host Computer Workstation
Buyers have the option of choosing a laptop or desktop computer as the host workstation. Whichever the case, this piece of equipment will have the computing power and processing muscle to handle high volume and high-complexity operations. The desktop host is an i5-6500 processor with 16 GB RAM and 2 Terabytes of storage with a 3-year warranty. The acquisition laptop option is a ThinkPad E580 running on an Intel Core i7 processor with 8GB RAM and 500GB of storage. These specifications, however, might be subject to change.
5-Year Warranty and Easy Payment Plans
Acquiring the equipment to run a veterinary and radiology service properly is a significant investment. It can be a hurdle for many trying to establish new offices or expand their current operations. To help clients acquire the equipment they need, they may choose between one-time payments or make reasonable monthly payments.
All the equipment that comes with this system is covered under a 5-year warranty, with 5-year drop coverage and software support included. The DirectVet Plus System offers peace of mind to all who choose to make it a part of their operation.
Take note that you may qualify for a deduction on capital equipment purchases under section 179 of the current Internal Revenue Service (IRS) tax codes. Your potential deduction might allow you to treat the full cost of new equipment and software as a deductible expense whether you purchase cash, capital lease, loan, or an Equipment Finance Agreement (EFA). Further information may be found on the IRS section 179 portal.
Final Thoughts
The DirectVet Plus Digital X-Ray System is an effective solution for veterinarians looking for a convenient, powerful, and user-friendly way to handle their x-ray needs. It is a system that doesn't need any additional power supplies, construction, or preparations. It is a self-contained veterinary digital x-ray equipment system that will be ready for use as soon as it's delivered, making it an excellent choice for veterinarians in the process of establishing their practice. Visit NewVetEquipment.com to place your order or have any questions or concerns you might have addressed.
Written by: Rachel Best
Treatment for Blocked Cats: The Power of Fluoroscopy
Urinary obstructions in cats are a life-threatening issue that vets see and treat commonly.
And while most vets have a system for caring for these unfortunate felines, it is exciting to learn about new technology that may provide value during the treatment of these critical patients.
One such development is fluoroscopy technology, which is now more accessible than ever to general practitioners. Here are three ways fluoroscopy may help while unblocking a cat…
Confirming Placement of the Urinary Catheter
Depending on the type of indwelling catheter used, it may be of value to check the placement of the catheter on radiographs.
This is especially true for red rubber catheters—which can double back on themselves or even tie into a knot if too much of the catheter is placed into the urinary bladder—or for any catheter long enough to cause additional trauma if passed so far that the tip contacts and irritates the bladder wall.
While traditional x-rays may be used for this purpose, fluoroscopy offers the advantage of being able to adjust the catheter placement in real time. That way, the catheter can be quickly adjusted prior to placing sutures.
Real-Time Contrast Studies of the Bladder and Urethra
Blocked cats with severely distended urinary bladders are at risk for bladder rupture—whether from the condition itself or from manipulation (pressure or cystocentesis) while the bladder is excessively full.
A large bladder rupture is often obvious since a full bladder will suddenly become difficult or impossible to palpate. However, a small tear or leak may be more difficult to detect.
A positive contrast cystourethrogram can help to identify small ruptures, by looking for contrast outside the borders of the urinary bladder on radiographs.
While traditional radiographs can certainly be used for this purpose, fluoroscopy may prove useful because of the ability to see things moving in real time, and the ability to move the patient and quickly see the abdomen at multiple angles without taking a lot of x-ray shots.
In addition to the bladder, this can be very useful for tracking the movement of contrast through the urethra (to identify obstructing materials, strictures, etc.), versus only seeing a couple of snapshots in time on traditional x-rays.
Since contrast media can be irritating to tissue that is already compromised, a vet must weigh the pros and cons of doing a contrast study right after unblocking a cat. But this procedure could also be useful after the cat has had time to heal, to ensure the bladder is intact before the urinary catheter is removed and the patient is sent home.
Evaluating for Uroliths and “Sludge”
In cats, sludge, sand, or gritty material—which may be a combination of crystals, blood clots, mucus, etc.—can accumulate in the urinary bladder. And while less common than in dogs, uroliths are sometimes diagnosed in cats.
On radiographs, sludge may be confused with a bladder mass or even sometimes with uroliths. Fluoroscopy can help with characterizing this material inside the urinary bladder (and distinguishing it from a bladder mass) by seeing how it moves in real time, as the patient is moved.
Additionally, a vet could use fluoroscopy to track the progress of flushing this material out of the bladder (or urethra) after relieving a blockage.
Conclusion
For many years, traditional radiographs have been included as part of the workup for blocked cats, and a vet can provide excellent care to feline patients with current protocols.
However, as fluoroscopy technology continues to evolve and become more accessible to general practitioners, it’s exciting to see the ways in which this modality can make a vet’s job easier and provide more information for patient care.
Written by: Dr. Tammy Powell, DVM
Planning and Measuring for Full-Body X-Rays
Full-body radiographs are a valuable diagnostic tool for well and sick veterinary patients alike.
Wellness screening, such as with a senior wellness package, may include full thoracic and abdominal radiographs in addition to bloodwork, as a screening tool to catch disease processes early.
And the use of full-body screening is widely recognized for ill patients—for example, as part of the diagnostic workup for patients with non-specific symptoms, when doing a “met check” to look for metastasis, or when evaluating the patient after a traumatic injury.
But how many views are required, and how are patient measurements performed when screening large portions of the body? These topics will be discussed below…
How Many Views Are Required?
Most experts recommend at least five views: right and left lateral thorax, VD thorax, lateral (usually right lateral) abdomen, and VD abdomen. For both the abdomen and the thorax, a DV view may replace a VD view in some cases, such as if a patient isn’t stable enough to lie in dorsal recumbency.
In general, this is considered the MINIMUM number of views by many veterinary radiologists. With that in mind, sometimes full-body studies require more than five views.
Here are some examples of additional views that may be needed…
Some experts recommend including BOTH a VD and DV view of the thorax, for a total of four thoracic views, especially when looking for metastasis or small/localized lesions.
More and more commonly, veterinarians are increasing their standard abdominal study to three views (adding a left lateral view as the third view), at least for GI studies. A left lateral is especially valuable for evaluating the pylorus.
For large dogs whose entire thorax or abdomen can’t be captured on the plate or sensor, they would require two of each of these views--a cranial and caudal portion for each view, so that each body cavity can be fully evaluated without any portion being cut off due to the patient’s large size.
Depending on what a practitioner is looking for, additional views (spine, limbs, skull, contrast studies, etc.) may be needed. This is especially true for blunt trauma, when the patient may have multiple injuries.
Is it possible to do a full-body study with less than five views?
Sometimes, this does happen. Everyone is probably familiar with the “cat-gram” (a lateral and VD view of a cat’s entire body, for a total of two views) that is commonly used in daily practice.
A vet will need to use their best clinical judgment for the needs of each individual patient, understanding that if less than the recommended five views are taken, details could be missed.
How to Measure a Patient for Full-Body X-Rays
Once the vet has decided which views are to be included in the study, this allows the vet team to measure the patient for each of these views.
The key is to measure the patient in the SAME POSITION they’ll be in during the study. This is important because the patient’s width may change with their position, thanks to the effects of gravity and the table and any props being used.
So, for lateral views, the patient should be lying on their side, for VD views they should be lying on their back… and so on.
Once the patient is in the appropriate position, a good rule of thumb is to measure them at the widest point for the area within the field of view. This is frequently toward the diaphragm/liver for both thoracic and abdominal studies.
This ensures the beam will be powerful enough to penetrate the part of the body being studied and produce a quality image.
However, there may be times when it makes sense to measure the patient using a different strategy, such as…
When focusing on a specific organ. For example, to see the most detail on the bladder, it would be helpful to measure that region of the abdomen. For full-body studies, this may be included in addition to the general screening shots.
If the patient’s body shape is such that measurements are significantly different at the widest and narrowest parts of the body within the field of view. In this case, two shots (at two different settings) may be necessary to see all fields at the right exposure and level of detail needed for diagnostic quality.
Full-body radiographs can be a great diagnostic tool that helps patients receive the care they need.
By using best practices and strategies, a veterinarian can ensure that these studies deliver the best possible diagnostic value.
Written by: Dr. Tammy Powell, DVM
What Is an Over-Exposed X-Ray, and How to Avoid Over-Exposed
An over-exposed radiograph is one in which the X-ray beam was too powerful, resulting in an excessively dark or “burnt-out” image.
Unfortunately, this can make it difficult or impossible to interpret the radiograph, which can lead to frustrating retakes or even non-diagnostic images.
Here are some important things to know about over-exposed X-rays and how to avoid them…
Why Are Over-Exposed Radiographs a Bad Thing?
Radiographs are about balance. A veterinary professional may feel like Goldilocks—wanting to avoid too few or too many X-rays passing through the patient and onto the film or sensor/plate, and instead, find the x-ray beam strength that is “just right.”
What happens otherwise?
Too few X-rays (or a beam that’s weaker) means an under-exposed (or whited out) image. Too many X-rays (a beam that’s too powerful) result in an over-exposed image.
In general, an over-exposed image may be more useful than an under-exposed image when working with physical X-ray films, thanks to the availability of hot light, an extra bright light that may allow a veterinarian to see more details when viewing an over-exposed film.
However, even a hot light can’t save a very over-exposed image. It’s always best to go for high-quality radiographs.
High-quality X-ray images are more diagnostic because they allow for the visualization of fine details that could otherwise be missed. For example, pulmonary vessels and small nodules might not be visible in an over-exposed radiograph.
How to Avoid Over-Exposed Radiographs
Improving the quality of radiographs involves troubleshooting. By figuring out WHY there is an issue with image quality, a veterinarian can most effectively improve their radiographs.
Here are some possible causes of over-exposed X-rays…
Machine errors. Sometimes, a generator, developer, or digital plate needs to be serviced in order to correct the problem.
An equipment issue may be more likely if ALL patient radiographs are showing the same issue, such as an exposure error. Keeping up with routine x-ray equipment maintenance can help to prevent this type of problem.
Technical errors. This is less common with digital machines that have preprogrammed settings.
However, it’s still possible, especially if the wrong part of the body has been selected for the study. Or, maybe the clinic has different sensors/plates with slightly differing sensitivities to the same exposure settings.
For film machines, errors in technique are common. Technique charts can help vet professionals select the best settings and reduce time-consuming retakes.
Either way, to obtain a lighter image, lower the kVp or mAs for the shot.
Operator errors. For film and digital studies alike, errors in measuring the patient are common. For example, when performing an abdominal or thoracic study, remember to take the patient’s measurement while they are lying on their side—this number could be surprisingly different from the patient’s width while standing up.
Also, the X-ray operator should remember to collimate the field. This improves the detail and reduces scatter radiation that could otherwise darken an image.
Training and practice can help veterinary team members master these protocols and obtain high-quality images.
Also, digital radiographs can help remove some potential human error (such as manually setting the technique) by automating much of the process.
Getting the exposure right the first time will help the whole team save time, reduce stress for patients and staff by avoiding frustrating retakes, and produce images of a higher diagnostic quality for excellent patient care.
Written by: Dr. Tammy Powell, DVM
Equine & Mobile Veterinary DR X-Ray with Wireless Panels
The Benefits Of A Mobile Veterinary X-Ray Service
When you work as a mobile vet, you are often faced with many challenging situations. Having instant access to X-ray technology helps a great deal when you are working in the field.
It does not matter if you are working with small or large animals, all vets find a mobile veterinary X-ray facility a useful tool.
For many mobile vets, veterinary digital X-ray technology has been out of reach both from a portability and cost point of view.
Thanks to advances in mobile X-ray technology, there is now a new player on the market. ExamVue offers mobile vets an opportunity to invest in mobile equine X-ray technology suitable for both field and clinic work.
What Is Included In The Package?
This easy to transport X-ray solution certainly has a lot to offer. The Wireless Portable DR system features a whole host of functions. It is suitable for both equine and other veterinary work.
The kit comes complete with a hardshell case specially made for the laptop and plate.
List of components:
Wireless laptop-based capture station
High-quality Cesium flat panel plate
A choice of plates - 14 x 17 or 10 x 12
Dedicated ExamVue Software
No cable is required between the plate and the laptop
The unique ExamVue PACS makes it easy to evaluate a case quickly. As a client, you will also benefit from a 5-year warranty along with 5-year dedicated phone support. Set up guidance and training as well as shipping and installation are included as part of the package.
Who Is This X-Ray Set up Suitable For?
This X-ray setup is suitable for both large and small animals. When you work with large barn animals, using X-ray technology as a diagnostic tool is often difficult. It often means transporting the animal to another location. Now you no longer need to do so.
The system does not need an electricity source. In other words, it works completely independently from the main supply of electricity. The focus is very much on self-sufficiency.
One of the main benefits of the system is that you don't have any cables to worry about when performing an X-ray. That makes entanglement and other hassle factors normally associated with portable X-ray equipment a thing of the past.
You can review your X-rays on site making an immediate clinical decision possible.
What Are The Benefits Of Csl Direct Technology?
As you will know, resolution plays an important part when making a diagnosis. This system offers excellent resolution thanks to its isotropic lateral scattering. You will also benefit from low photon coupling loss which means better quantum efficiency and detector quantum efficiency.
The Wireless Flat Panel
The wireless flat panel offers you the latest in mobile veterinary X-ray tech including minimal exposure time. High sensitivity and resolution are important for reliable diagnosis and image quality.
Thanks to the excellent image quality, patients will receive a lower dose of radiation without the need for several X-rays.
The plates are structured in such a way that they are protected from degradation due to moisture. Good durability thanks to the Csi:TI screen. Your choice of panel is delivered in a flat panel case for easy storage and handling.
Software Performance
The ExamVue DR software is both easy to learn and use. It is one of the few equine X-ray software programs that feature processing, storage, acquisition capture, and the viewing of digital images.
To date, ExamVue has been used in a range of X-ray disciplines including orthopaedic and podiatry. The interface makes the software easy to learn for both experienced and novice vets.
Other software functions include printing, CD - DVD burn, image stitching, and procedure mapping. You also have a facility that allows you to create worklists.
Above all, ExamVue offers excellent value both in terms of functionality and cost-effectiveness.
Other Software Features That Will Impress You
Looking at the software in more detail, you will find that it also offers many other features.
This is a guide to other features you will find useful:
Console Acquisition Software
Patient registration facility using a manual function of Dicom worklist.
Complete processing parameters from small to large.
Edge enhancement function, histogram and contrast.
You can review images by horizontal and vertical flips.
The software lets you rotate images both clockwise and counter clockwise.
Complete zoom and pan along with a magnifying and crop facility.
The software has a field for annotations and measurements for free text and arrow markers.
Backed up by Cobb's and Norberg Angle Measurement.
Image preview facility
The emergency mode allows an examination without patient data input.
Facility for sending Dicom print to a Dicom printer
Dicom storage along with hard disk capacity notification function.
Exportable image facility which includes PNG, JPG, BMP, and Dicom to other forms of media. No viewer is required.
Database function that allows side by side images and a list of other functions including repeat, delete, and reject.
Gridline removal function and stitching software
Comes complete with AED mode ( Automatic Exposure Detection) which does not require connection to the X-ray generator.
Laptop Details
The laptop that comes as part of the package is a Dell Wireless 1506. It benefits from a 15.6" HD screen with wide-view anti-glare capability. The operating system is Windows 10 and it features 8 GB of RAM.
The package is backed up by Intel Integrated HD graphics 4400 featuring a 500 GB hard drive. The ExamVue Software is preloaded on delivery of the laptop to you.
That is good to know when you are thinking about investing in a mobile veterinary X-ray facility. For more information, you can contact the company and further familiarize yourself with their range of other veterinary product lines.
https://newvetequipment.com/dr-wireless-system
Written by: Annie Wall
Diagnosing Dental Disease in Small Mammals: A Vet's Guide
Since dental health can be a serious issue that affects a pet’s ability to eat, it’s important to address dental disease when it arises—even in the smallest of patients, like small mammals or pocket pets. While these tiny mouths can be challenging to work with, it is possible to evaluate and treat dental issues in these species.
In recent articles, we’ve discussed dental care in rabbits and guinea pigs. Today, we’ll focus on small rodents such as hamsters, gerbils, mice, and rats.
Which Dental Issues Do Small Mammals Develop?
These species (gerbils, hamsters, mice, and rats) can develop incisor malocclusions, since their incisors are open-rooted and grow continuously.
Unlike rabbits and guinea pigs, these small rodents have closed-rooted molars that do not grow continuously. Fortunately, that means that dental issues of the cheek teeth, while possible, are much less common.
On the other hand, since their molars have fully developed roots and don’t continuously erupt, small rodents may develop periodontal disease secondary to plaque. They may also develop dental caries if fed a diet heavy in sugar, including excessive use of certain commercial rodent treats.
Other oral issues include trauma to the teeth or jaws, food impaction, abscesses and infections, or diseases such as neoplasia. In hamsters, cheek pouch eversions or impactions are especially common.
Normal Dentition in Small Mammals
Mice, rats, gerbils, and hamsters have the dental formula 2(I 1/1, C 0/0, P 0/0, M 3/3), for a total of 16 teeth, with a space called the diastema between the incisors and molars.
The mandibular incisors are about three times as long as the maxillary incisors. The enamel may be white to yellow or orange, depending on the species.
As mentioned above, their incisors grow continuously, while their molars do not.
This dentition is consistent with the lifestyle of these small exotic pets. Their diet primarily includes seeds, roots, tubers, and grains—so unlike rabbits and guinea pigs, they don’t ingest a lot of fiber to the point where they require continuously erupting cheek teeth.
Their incisors wear down due to gnawing and burrowing behaviors. Chewing aids—such as wooden blocks or cardboard that is free of print or dyes—can help promote this natural behavior and keep the incisors in good shape.
Diagnosing Dental Disease in Small Mammals
Symptoms may be subtle at first, and it is common for pet owners to miss disease until it becomes more advanced. Symptoms may include anorexia, any change in behavior (such as hiding or hunching if they are in pain), drooling, and swellings or changes to face symmetry.
Hamsters with cheek pouch impactions may present with swollen cheeks. Or the cheek pouches may be seen protruding from the mouth in the case of eversions.
It’s possible for a veterinarian to do an initial, cursory oral exam on an awake pet using an otoscopic cone, and to evaluate the incisors on an awake pet. This method may uncover obvious abnormalities. But it is likely to miss subtle changes and does not allow for a thorough oral exam.
Anesthesia or sedation are best, both for a full oral examination and for dental radiographs.
Additional tools for small rodents, such as mouth gags and cheek retractors, are needed to get the best view of the teeth and oral cavity. Magnification can also be very valuable.
A dental x-ray study is best performed using a dental x-ray unit, with the sensor placed extra-orally due to the small size of these patients. Mammography film can also be used, as it shows fine details.
Treating Dental Disease in Small Mammals
For incisor malocclusions, the goal is to restore the teeth to their normal length and function. An appropriate type of dental drill is recommended. Avoid nail trimmers, rongeurs, and other cutting tools as these carry a risk of fracturing the teeth during trimming.
Molars should NEVER be trimmed since they have true roots and don’t erupt continuously. However, these cheek teeth may require removal of tartar and treatment of periodontal disease or even extraction of severely diseased or abnormal teeth.
For hamsters with cheek pouch eversions, viable tissue should be put back into normal position and sutured to the cheek. With impactions, the pouch must be emptied out and rinsed with saline.
Antibiotics and pain medications should be prescribed as needed, depending on the pathology.
Any vet treating dental disease in small rodents must have the appropriate sizes and types of dental tools. It’s also possible to use a needle (18 to 25-gauge, depending on the size of the patient) as an elevator during extractions.
Appropriate training is also very important, to ensure these small patients receive the specialized care their need.
Due to their fast metabolism, nutritional support is usually needed until the animal is recovered and eating on its own.
Owner Education is Important
Many clients buy these small pets for their children and don’t necessarily interact with the pets on a daily basis or have a deep understanding of their husbandry needs.
Promoting regular checkups of these patients can help to catch issues early, as well as educate owners on husbandry and on how to tell if their pet is ill.
All of this can serve to better the health of these small rodents and help to catch dental disease or other health issues early, when treatment may be simpler and carry a better prognosis.
Written by: Dr. Tammy Powell, DVM
Essential Guide to Guinea Pig Dental Care
Guinea pigs have teeth that grow continuously, and their dental needs are very different from the dental needs of a dog or cat.
However, dental health is still a vital part of a guinea pig’s wellbeing. Here are some important things to know…
Which Dental Problems Do Guinea Pigs Develop?
Congenital malocclusions are possible in guinea pigs, although much less common than in rabbits since guinea pigs have not been bred with dwarf or shortened snout variations.
Acquired dental disease accounts for the majority of dental issues in guinea pigs—with dietary factors being a primary cause, due to uneven or inadequate wearing down of the teeth.
A common problem is an inadequate fiber in the diet, which is normally provided via hay. A vitamin C deficiency can also lead to dental issues since it affects the integrity of the connective tissues that hold the teeth in place—leading to loose and misaligned teeth and subsequent tooth overgrowth.
Any other local or systemic issues (trauma to the jaws or teeth, systemic disease, neoplasia, etc.) that affect a guinea pig’s eating habits could also lead to dental problems.
The uneven or inadequate wearing of the teeth can cause malocclusions, elongated crowns, and sharp edges that can injure or ulcerate the buccal mucosa and cause pain. Overgrowth on the lingual aspect may entrap or irritate the tongue. All of this can make it difficult or impossible for a guinea pig to eat.
Abscesses or infections may also occur, although this is much less common than in rabbits.
Normal Guinea Pig Dentition
In order to recognize what is abnormal in this species, it’s important to know what’s normal for them.
Guinea pigs have open-rooted teeth that continuously grow, and they wear down their teeth by chewing on fibrous foods.
Their dentition is the same in all four quadrants: one incisor, followed by one premolar and three molars. Guinea pigs do not have canine teeth, but instead have a space called the diastema between the incisors and the premolars.
The premolars and molars are anatomically identical and collectively known as the cheek teeth.
Since the mandible is wider than the maxilla, the cheek teeth curve (the mandibular teeth inward and the maxillary teeth outward) to occlude with one another on a sloped plane.
Signs of Dental Disease in a Guinea Pig
Since guinea pigs are prey species, they try to hide signs of a problem for as long as possible. But a pet owner may pick up on changes in eating habits, which develop even in the early stages of malocclusions.
Anorexia is a common symptom of dental problems.
Other symptoms may include weight loss, changes in fecal output (quantity and appearance), dropping food, changes to grooming habits (and subsequent skin issues), salivation, and GI stasis. Facial swellings are possible but less common.
Diagnosing Dental Disease in Guinea Pigs
General anesthesia is best for a thorough dental evaluation.
Cheek teeth abnormalities are very common, more so than incisor malocclusions. So, if an incisor malocclusion is present, it’s a good indicator that a closer look at the cheek teeth is necessary.
A visual examination with a good light source and an otoscopic cone or speculum may reveal a dental issue. However, small or subtle lesions can be missed this way.
Use of an endoscope is very helpful for diagnosing dental problems in guinea pigs, with the added bonus of clear images to show clients so they truly understand the issue.
Radiographs are also important for diagnosing dental issues. And if available, CT is an excellent tool for obtaining diagnostic information.
Treating Dental Disease in Guinea Pigs
Supportive therapy is usually needed, since dental problems impact a guinea pig’s ability to eat, and pets may present in poor condition with weight loss and anorexia. Supportive care commonly includes fluid support, dietary support with a critical care formula, and pain relief.
All of this can help stabilize the patient for anesthesia, prevent complications such as GI stasis, and promote a better recovery and return to normal eating habits.
The main goal of dental treatment is to restore the normal length and shape of the teeth as much as possible and to promote normal occlusion in the process.
A high-speed dental drill is generally used while cutting tools are not recommended because they can cause fractures in the teeth. If needed, extractions of diseased teeth or surgical removal of abscesses can be performed, along with appropriate antibiotic therapy.
Prognosis varies, based on the severity of the disease. Severely overgrown teeth may require multiple treatments are done 1-2 months apart, or even chronic palliative treatments.
To perform safe and effective dental procedures for guinea pigs, it’s important for a veterinarian to gain training and experience, and to have the right tools. Referral to a specialist is a good option, too.
Prevention Is the Best Medicine
Since most dental problems in guinea pigs are related to diet, client education can go a long way toward preventing dental issues in guinea pigs.
Providing instruction on a guinea pig’s dietary requirements is a great step at a new pet visit. Additionally, owners should know to look for anorexia or changes in their pet’s eating habits and to report concerns to their vet right away.
Quick recognition of a problem could help to catch the issue early, resulting in more timely and effective treatment
Written by: Dr. Tammy Powell, DVM
Essential Rabbit Dental Health Tips for Better Teeth
Although rabbits don’t undergo regular dental cleanings the way dogs and cats do, dental health is still an extremely important part of a rabbit’s wellbeing. When dental problems occur, a rabbit might be unable to eat or drink.
For a veterinarian to provide rabbit dental care, it helps to know which dental problems this species is prone to, how to treat them, and how to prevent dental issues with home care and client education.
Which Dental Issues Do Rabbits Develop?
A rabbit’s teeth grow continuously throughout its whole life. As such, tartar isn’t really a problem the way it is in dogs and cats.
An appropriate diet—with the right nutrition and plenty of roughage—plays a crucial role in wearing down the teeth naturally, so that they don’t overgrow.
In fact, many rabbit dental issues are due to husbandry concerns. An inappropriate diet is most common.
Other acquired dental conditions include broken teeth, jaw fractures and other trauma, oral foreign bodies, metabolic bone disease (which can also be nutrition-related, or due to a vitamin D deficiency in indoor rabbits), and any systemic disease that affects a rabbit’s ability to eat and therefore keep their teeth in good shape.
Overgrowth of the teeth can lead to sharp edges, as well as malocclusions that make it difficult or impossible to eat. Infections and abscesses (in which the purulent material turns very thick) can also occur.
While acquired dental problems are very common, congenital issues may also play a role. This may include malformations of the jaws or of the teeth themselves.
Normal Rabbit Dentition
To properly diagnose and treat rabbits, it’s important for a veterinarian to know what is normal for this species.
Rabbits have four maxillary incisors (two large teeth, plus a pair of smaller “peg teeth” directly behind them) and two mandibular incisors. They do not have canine teeth—instead, there is a space called the diastema.
Following the diastema, the cheek teeth are made up of three premolars and three molars on each side of the maxilla, and two premolars and three molars on each side of the mandible.
Since malocclusions are common, it’s also important to know the normal occlusions in a rabbit.
The mandibular incisors occlude just between the two sets of upper incisors.
The mandible is narrower than the maxilla, so the upper cheek teeth are not normally in contact with the lower cheek teeth. Effective chewing of hay and other fibrous foods comes from a grinding motion of the cheek teeth.
Diagnosing Dental Disease in Rabbits
A change in eating patterns is often the first sign of a problem.
Other symptoms may include fecal changes (quantity and appearance), bruxism, drooling, decreased grooming, weight loss or a general decline in condition, and other symptoms localized on the face (swellings, nasal discharge, epiphora, exophthalmos).
A full dental examination is best performed under sedation or general anesthesia. A metal speculum or otoscope cone with good lighting will aid in the visualization of the cheek teeth. An oral endoscopy is an excellent option, if available.
A veterinarian should look for misshapen teeth, sharp edges, malocclusions, and anything else that can interfere with a rabbit’s ability to chew. Also, look for swellings or other abnormalities of the mouth or jaw.
In addition to the physical examination and dental evaluation, skull radiographs can provide crucial information about the extent of the disease and prognosis, which can contribute to making a treatment plan.
Blood work can help rule out other conditions and ensure the rabbit is healthy enough for a dental procedure under anesthesia.
Treating Dental Disease in Rabbits
The teeth must be returned as closely as possible to their original length, alignment, and ability to function.
This means overgrown teeth must be shortened to their normal length, and normal occlusion must be restored. This could be done in one procedure, or via multiple procedures over time for patients with more extensive abnormalities.
Diseased or severely overgrown or malformed teeth may need to be extracted, although extractions of cheek teeth are ideally kept to a minimum.
Additional ailments, such as abscesses, must also be treated—which in rabbits often means surgical resection and antibiotics.
Familiarity and practice are required to perform these procedures, as a rabbit’s mouth is very different from a dog or a cat.
It’s a good idea for general practitioner veterinarians to gain training in rabbit dental care before attempting complex procedures. It’s also crucial to have the right tools for a rabbit’s teeth.
Referral to a specialist is also an option, either after the diagnosis is reached, or at the rabbit’s initial onset to the clinic. But general practitioners with the right training and appropriate tools at their practice may be able to treat some rabbit dental conditions themselves.
Either way, earlier treatment is best, both for the dental prognosis and for the rabbit’s overall health, since their condition can decline quickly if they have difficulty eating. Nutritional support may be needed until the patient is able to eat on their own.
Owner Education Is Necessary to Prevent Recurrence
Remember to talk to the owner about husbandry—including a proper diet with the right balance of nutrients and fibrous materials for tooth health.
Dental treatment is only a short-term solution. Addressing the underlying cause (which is often husbandry-related) is the only way to prevent the issue from happening again.
Written by: Dr. Tammy Powell, DVM
Essential Oral and Beak Care for Birds: A Guide for Vets
Even though birds don’t need the same type of oral or dental care that dogs and cats do, their oral and beak health is still an important part of their wellbeing.
Many avian patients are not only beautiful, they are also very intelligent, with big personalities. As such, many veterinarians enjoy seeing birds at their practice. However, to appropriately evaluate and treat these patients, extensive knowledge is required of the many differences between birds and mammals.
While it won’t be possible in just one article to cover every issue a bird could have with its mouth or beak, below we’ll cover some of the most common conditions to look for in pet birds, mostly focusing on Psittacines (parrots).
Normal Anatomy and Signs of a Problem
The beak is also known as the bill or rostrum. It consists of the upper (maxillary rostrum) and lower (mandibular rostrum) jaws, each of which is covered at its rostral end by a hard keratin structure known as the rhampotheca or “horny bill.”
Normally, the upper and lower portions of the beak should align well with one another. But various beak or systemic health problems can lead to overgrowth, malocclusions, or other problems. Additionally, health issues can present within a bird’s mouth.
An owner may alert their veterinarian to a problem by mentioning symptoms they’ve noticed at home, such as halitosis, yawning, frequent beak rubbing, or changes in eating behavior.
During the physical examination, keep a lookout for any asymmetry of the head and beak. Look inside the mouth for lesions, too, such as masses, plaques, odor, foreign bodies, or wounds.
When examining a bird, a low-stress approach is best—for the ease of the veterinary visit, for avoiding spurious lab results due to stress, and for the wellbeing of the bird. Avoid using excessive pressure or restraint. For some birds, sedation may be ideal.
Common Health Conditions of the Beak and Mouth in Birds
Some of the most common conditions a veterinarian will see include…
Beak overgrowth, uneven wear, or malocclusions. Routine beak trimmings can help prevent these problems. Commonly, a Dremel is used for this purpose. It can take practice and experience to gain proficiency. The Dremel should not be held in contact with the beak for too long, due to the risk of excessive heat.
More complicated issues, such as a malocclusion, may need additional treatments or referral to a specialist.
Once the beak shape is corrected, enrichment at home, which encourages normal use of the beak, can help prevent the problem from occurring again and possibly eliminate the need for further beak trimmings.
Beak and oral trauma. Common traumatic injuries include bite wounds/punctures (from other birds or other animals), fractures (which may be just to the tip of the keratin part of the beak, or may involve underlying bone), avulsions, and oral trauma or punctures from hard objects or toys.
Oral and beak diseases. Birds may suffer from bacterial, fungal, viral, and parasitic infections. One example is the viral Psittacine Beak and Feather Disease. Also, neoplasia may occur.
Systemic diseases can also affect the beak or oral cavity. One condition which may affect the mouth and GI tract is an internal papillomatous disease (IPD). Psittacines with this condition may present with cauliflower-like growths in their oral cavity or cloaca, while also having masses present internally.
An overgrown beak may be an indication of malnutrition or systemic disease (such as liver disease).
And Candidiasis (thrush) may be an indication of an underlying disease or immunosuppression.
Diagnosing and Treating Beak and Oral Health Conditions in Birds
In addition to symptoms reported by the owner and physical exam findings, diagnostic tests are often indicated. This could include radiographs to evaluate the extent of an injury, bloodwork to look for systemic disease, infectious disease testing, histopathology of masses or growths, or other testing as needed.
Treatment depends on the diagnosis. In some cases, a simple beak trim with a recommendation for home enrichment may be all that’s required. With certain diseases and injuries, the treatment may be much more complicated.
Depending on a veterinarian’s knowledge and comfort level with birds, they may consider referral to a specialist. Knowing the common oral and beak conditions in birds, what to look for, and what is normal versus abnormal anatomy, can help a practitioner know when a referral is warranted.
For any veterinarians wishing to care for more birds at their practice, continuing education, hands-on labs, practice/experience, and good informational resources can all help with developing the knowledge and skills needed to evaluate and treat these beautiful and unique patients.
Written by: Dr. Tammy Powell, DVM
Veterinary Dental Cleaning Techniques in Dogs
Dogs come in many shapes and sizes, but all of them can be affected by dental and periodontal disease.
Here are some important things to consider for dental cleanings in dogs…
What’s the Normal Dentition for a Dog?
While it’s important to recognize what’s abnormal, it’s just as important to know what’s NORMAL when it comes to a dog’s teeth.
For example, many clients ask questions like ‘how many teeth does a dog have?’. A quick and confident answer can help instill confidence in the veterinarian’s knowledge.
Also, during a dental procedure, knowing the expected number of teeth will help a vet know if any teeth are missing—an abnormal finding that warrants further exploration and dental radiographs.
It also helps to know how many roots each tooth has, as well as the approximate length and direction of each root. That way, a vet can plan for the most efficient way to extract a tooth, and it will be less likely that any root tips are left behind.
What Are the Most Common Dental Issues in Dogs—and in Specific Breeds?
Periodontal disease is, of course, very common, affecting more than two-thirds of dogs by three years of age.
But while any breed can be affected, certain breeds are more prone to developing tartar and periodontal disease quickly. Often, this happens to small or brachycephalic breeds due to tooth crowding.
Big dogs, on the other hand, maybe more likely to suffer traumatic tooth fractures.
While it’s important to keep a lookout for anything that could be part of a disease process, knowing the common issues in each size and breed of dog could help a vet know where to look for issues and pick up on subtle or early changes.
When Should Dental Radiographs be Taken?
Dental radiographs are considered the standard of care for dental procedures. Some estimates state that dental x-rays can reveal about 40% more pathology than can a visual oral examination alone.
This leads to better patient care. Also, the x-ray images can help clients visualize their dog’s dental health status and therefore better understand the importance of the treatments a veterinarian recommends.
So, when and how should dental radiographs be performed?
Many experts recommend taking a full set of dental radiographs immediately after anesthesia induction. Usually, this task is performed by a skilled vet tech or nurse, along with anesthesia monitoring.
Performing radiographs prior to the cleaning gives the vet a chance to review the radiographs. These findings, along with a visual assessment of the patient’s mouth (including charting), gives a lot of information to support a call to the owner, if needed for additional treatments.
Some veterinarians prefer to do radiographs after the dental cleaning is performed, so they can first remove large chunks of calculus that could interfere with radiographic interpretation. There’s nothing wrong with this, and every practice should do what works best for them.
The most important thing is probably to have a consistent protocol, to improve efficiency.
It’s worthwhile to invest in training for this important skill. Consider sending team members to a conference or course, or asking the company that sold the dental x-ray equipment if they offer training.
Since dogs differ greatly in size, it helps to have more than one size of film/plate/sensor available. In order to be diagnostic, x-ray images must show 2-3 mm of bone from the apex of the root. The crown of the tooth doesn’t necessarily need to be included.
For routine cleanings, one set of radiographs may be all that is needed. But for patients who are receiving extractions or more advanced procedures, it’s beneficial to perform post-op dental x-rays. This confirms that everything was done properly and safely, in case any new concerns arise later.
Tips for Cleaning a Dog’s Teeth During a Dental Procedure
After radiographs and charting are finished, the typical dental procedure consists of scaling and polishing.
Here are a few tips for the dental cleaning:
Scaling of the enamel, above the gumline, can be done with an ultrasonic/and or hand scaler.
It’s recommended not to spend more than 10-15 seconds on a tooth with the ultrasonic scaler, to avoid overheating and damaging the tooth.
Subgingival cleaning may be performed by hand, or via a special “subgingival tip” on the ultrasonic scaler that is designed to be used on a lower setting and is less prone to overheating the tooth. For simple dentals without significant gum recession, this may be all that is needed.
If using ultrasonic scalers, many experts recommend following up with hand scaling for more detailed work or hard to reach places, to ensure no tartar is left behind.
For periodontal pockets ranging from 3-5 mm with no other pathology (mobility, etc.), closed root planing and subgingival curettage may help to reestablish the health of the pocket and soft tissue attachments to the tooth.
For pockets deeper than 5 mm where the tooth is being treated (rather than extracted), open root planing is recommended. Referral to a specialist may be best.
It’s important to stock tools in different sizes to accommodate different breeds of dogs. Having the right tools can make a veterinary team member’s life much easier and allow them to more easily reach and clean crevices or tight spots.
Due to the prevalence of periodontal disease, there’s no doubt that dental health is important for a dog’s wellbeing.
Client expectations are evolving. Many devoted pet owners research dental procedures online and expect a high level of care for their dog’s oral health needs.
By investing in dentistry—and then communicating the value of each step to their clients—a veterinary practice can bring in income while providing excellent care to their canine patients.
Written by: Dr. Tammy Powell, DVM
Stainless Steel Wall-Mounted Folding Exam Table
The New Vet Equipment stainless steel wall-mounted folding exam table is an economical option to many other tables on the market with its cost-effective construction and mounting system.
This wall-mounted exam table folds up for easy storage when not in use. Its versatility also allows it to be used for various applications in a healthcare facility, such as for recumbent patient access or as a transfer device.
Sturdy support
The steel folding exam table is made of stainless steel and has a weight capacity of 120 pounds. The exam table can support up to 44 inches wide and 24 inches deep, making it ideal for various medical facilities.
Many medical departments already have exam tables in their facilities, but some need a new one. By investing in this table, you're getting a quality product that can be used for many years to come!
Foldable
The user can simply fold the table upwards, which will make it nearly vertical to the wall. You can easily fold up the table and store it in a corner or closet when you're not using it. It's made of high-quality materials and is thin, so it can't take up too much space.
That way, you have extra room to do whatever you want without it getting in your way!. The table weighs roughly 44 pounds and stands 5 feet tall when folded.
Hygienic
This product is rust-resistant, making it a durable option for any facility that needs an exam table. The steel folding exam table is also easy to clean, so you do not have to worry about any unwanted diseases or infections spreading around your facility.
Good for small spaces
This product can be used in small clinics and offices where space is limited or patients need immediate treatment without waiting rooms.
Free delivery
Each exam table will arrive at your facility ready to be assembled in just minutes. Therefore there is no need for special tools such as screwdrivers or hammers to assemble this product.
Easy assembly
All parts can be easily moved and organized without any tools other than your hands. It works well for many different purposes. It's great for hospitals, clinics, and doctors' offices. It's also great for physical therapy, massage and acupuncture patients, and more.
The benefits of stainless steel tables in healthcare are numerous. And they can be the difference between having a functional medical facility or not. Stainless steel is the best choice because it is:
Durable - Stainless steel is a solid and durable material that will last for many years. It won't need to be replaced like a wooden table might.
Appealing - Stainless steel tables and equipment have an attractive, modern look perfect for any healthcare environment.
Infection Control - Stainless steel provides a safe surface for patients and healthcare professionals to work with. Easy to clean, stainless steel reduces the risk of infection from harmful bacteria and viruses.
Functional - Stainless steel is sturdy and durable and lightweight enough to move easily when necessary. This durability makes it a great option for hospitals or other medical facilities where equipment needs to be moved frequently.
Takeaway: The New Vet Equipment stainless steel wall-mounted, folding exam table can be used in outpatient clinics or physical therapy offices of all kinds.
Written by: Rachel Best
Upgrade Your Practice: Burton Veterinary LED Exam Light
The Burton Veterinary LED Exam Light is the ultimate tool for any professional looking to improve the quality of their practice. The fixture provides an excellent 90 000 lux at 30" from the bulb, making it one of the brightest LED lights on the market today. It uses a 3-chip LED array with a CRI of 95, producing a broad spectrum for veterinary examinations.
Designed for Pet Comfort
The Burton Veterinary LED Exam Light is the next generation of high-density, energy-efficient, cost-effective illumination for veterinary clinics.
The light's unique design provides a warm, natural color and a soothing effect for pet patients. The high-definition lens diffuses the light to produce a shadowless examination field and eliminates the need for mirrors or reflectors.
Heat Free
This product improves patient care by providing brighter, more intense illumination with less heat to minimize thermal tissue damage.
By delivering highly focused light for a longer duration than traditional incandescent lamps, our torches provide a greater field of vision for surgeons and dental professionals. The heat-free light guarantees 75% energy savings over the current halogen option.
Lighting Efficiency
The new LED is the brightest, most energy-efficient light in its class. Producing 90,000 lux at 24″ (61 cm).
The LED light uses 20% of the energy used by conventional fluorescent lights while being 25% brighter and lasting longer.
The LED light delivers a uniform, shadow-free field of light. The fixture produces a more balanced field of light with less contrast at the cost of some brightness. A separate cold filter reduces room ambient and provides optimal color temperature for viewing under magnification.
3700 k Color Temperature
With the 3700k color temperature and the ability to light up to 3 inches, you'll be able to get the job done better than you ever have before! Animals are a lot more comfortable with this light, allowing you to examine them in a more efficient, easier way.
This light will last you a very long time, reducing the amount of money you spend on veterinary equipment and increasing the comfort of the animals living in your care.
CRI (Color Rendering Index) of 95
The Burton LED Exam Light improves upon the old-fashioned bulb-type exam lights with a CRI (Color Rendering Index) of 95, which makes the colors of the animals' skin appear more accurately.
This is especially helpful when examining animals with light-colored fur like kittens! The LED light doesn't feel hot like a bulb light to be less scary for the animal.
High Rg>87 that can accurately capture different skin tones
The Burton Veterinary LED Exam Light was designed to excel in veterinary care. Not only does it provide dermatologists and veterinarians a dependable and easy-to-use light source, but it also provides a warm and uniform illumination for a spot or indirect examination. With the Burton Veterinary LED Exam Light, skin tones are captured as they are, with full detail and accurate representation.
It is designed to rotate 360 degrees and can be positioned up to 37.5 inches away from the patient (body part) on which it's being used! This product has an average life span of 20,000 hours.
This particular model is dimmable, but it comes equipped with an efficient switch that allows you to change the strength of the intensity. It is easy to clean and features antimicrobial paint that keeps it sterile.
Takeaway: Burton Veterinary LED Exam Light is proven to increase diagnostic accuracy. Get yours today!
Written by: Rachel Best
Essential Tips for Feline Dental Health: Best Practices
As a veterinarian, you already know how important dental health is to your patients—and you also know that dental health concerns can vary by species.
Today, we’ll be covering some tips for dental care in cats, both before and after the dental procedure.
Knowing Your Way Around a Cat’s Mouth
Quick—how many teeth should an adult cat have?
Clients often ask questions like this. A timely, confident answer will help inspire confidence when they leave their pet with you for oral care.
Plus, knowing the normal dental formula for each species serves an important purpose DURING a dental procedure.
For example, it helps a veterinarian or vet tech easily determine whether or not there are any missing teeth—a discovery that could prompt further exploration and potentially diagnose a problem that needs to be addressed.
Similarly, when performing extractions, it’s important to know how many roots the tooth has, to ensure no root tips get left behind. Knowing the approximate length and direction of each root will also help a vet extract the tooth more efficiently.
Know the Most Common Issues to Look For
Of course, dental tartar and periodontal disease are common concerns in both dogs and cats. But each species also carries their own unique dental problems that occur commonly.
For example, FORLs/resorptive lesions are fairly common in cats, but not so much in dogs. Felines are also more prone to certain inflammatory conditions such as stomatitis.
While it’s important to keep a look out for anything that could be part of a disease process, knowing the common issues in each species could help a vet pick up on subtle or early changes.
Also, be aware of normal structures that could be confused for a mass or lesion—such as the lingual molar salivary gland in cats.
Dental Radiographs: Why, When, and How
The WHY is simple: Dental x-rays are important because they allow a veterinarian to see the whole picture of a pet’s dental health—which frequently includes problems brewing below the gumline.
But, WHEN and HOW should dental x-rays be performed?
Many experts recommend taking a full set of dental radiographs immediately after anesthesia induction. Usually, this task is performed by a skilled vet tech or nurse, along with anesthesia monitoring.
It’s worthwhile to invest in training for this important skill. Consider sending team members to a conference or course, or asking the company that sold the dental x-ray equipment if they offer training. And setting up a standard technique (performing the views in the same order each time) can improve efficiency.
Performing radiographs prior to the cleaning gives the vet a chance to review the radiographs. These findings, along with a visual assessment of the patient’s mouth (including charting), gives a lot of information to support a call to the owner, if needed for additional treatments.
For routine cleanings, this may be all that is needed. But for patients who are receiving extractions or more advanced procedures, it’s beneficial to perform post-op dental x-rays. This confirms that everything was done properly and safely, in case any new concerns arise later.
Tips for Cleaning a Cat’s Teeth During a Dental Procedure
After charting is done, the typical dental procedure consists of scaling and polishing.
Scaling of the enamel can be done with an ultrasonic/and or hand scaler, while curettes (sometimes in combination with a specialized, “periodontal tip” on the ultrasonic scaler) are used to clean below the gumline.
Polishing is performed using a low-speed handpiece, usually with disposable prophy angles and fine-grit prophy paste.
Dental extractions may be done at the point during the procedure that works best for that patient’s needs and the veterinarian’s preference. For example, it may make sense to pull very loose teeth prior to cleaning (no point in spending time cleaning a tooth that is about to fall out), while more complicated extractions might be performed further into the procedure.
Here are a few tips for dental cleaning:
Make sure to stock the right size tools (scalers, etc.) in the practice, which means a range of sizes if you see everything from cats to large dogs. Smaller tools for cats allow for getting into crevices and cleaning more efficiently.
Use time limits to avoid overheating of the teeth, i.e. no more than 10 seconds at a time on any tooth with the ultrasonic scaler, or 5 seconds with the polisher.
In cats, due to the small size and shape of their skull, the eye sits very close to the maxillary teeth. Therefore, be careful while probing or cleaning deep periodontal pockets in that area (not to mention during nerve blocks or extractions) to avoid traumatic injuries to the eye.
Due to the prevalence of periodontal disease, and the abundance of oral and dental diseases that can occur in cats, there’s no doubt that dental health is important for their overall health and comfort.
Client expectations are evolving. Many devoted pet owners research dental procedures online and expect a high level of care for their cat’s oral health needs.
By investing in dentistry—and then communicating the value of each step to their clients—a veterinary practice can bring in income while providing excellent care to their feline patients.
Written by: Dr. Tammy Powell, DVM
8 Things to Know about Being the Spouse of a Veterinarian
So, you married a veterinarian…
Veterinarians usually don’t work a 9-to-5 job, and the unique demands of their career may sometimes interfere with home life. Not to mention, your spouse may come home talking about weird things like abscesses and parasites.
Here are some things to consider when it comes to understanding and supporting your partner…
1. Veterinary Medicine Tends to Attract Empathetic, Caring Individuals
For a job that pays less than their human medicine counterparts, along with long hours and other demands of a vet’s day, it’s safe to say that veterinarians are definitely not in it for the money.
Instead, clinical practice veterinarians typically choose their career because they love animals and want to help them. These caring individuals have big hearts and give a lot of themselves in the process of caring for their patients.
Maybe these are some of your favorite qualities about your partner.
2. But, All That Caring Can Take a Toll…
Because veterinarians care so much about their patients, it’s easy for them to experience an emotional roller coaster each workday, as some patients have happy visits while others may be severely ill or euthanized.
This can lead to compassion fatigue, where a person begins to feel burnt out and drained due to the emotional impact of their work. Compassion fatigue, along with many other factors unique to working in veterinary medicine, contributes to the fact that veterinarians have a higher suicide rate than many other professions.
While this can be scary, awareness goes a long way toward supporting your spouse.
You can help them by lending an ear or a shoulder to cry on when they need it after a tough day, by helping them find a psychological professional to talk to, or by referring them to a helpful resource such as NOMV (Not One More Vet) or Vets4Vets.
The National Suicide Prevention Lifeline (1-800-273-8255, or text “Home” to 741741) is also a life-saving resource.
3. Many of Veterinarians are Introverts
While there are also extroverted vets, being an introvert is a common trait when it comes to veterinarians.
And yet, a veterinarian’s job involves a lot of interaction with people—both coworkers and lots of clients during a busy day.
For this reason, your partner might not always be up for social events after work. They may need time alone to rest and recharge.
If this sounds like your spouse, remember that they aren’t avoiding people to be difficult or limit your social life. Instead, they may just need to “refuel” before they’re ready to be social.
4. Vets Often Work Long or Irregular Hours
This can create logistical challenges for tasks such as picking up the kids from school.
And a vet may be reluctant to make plans for right after work, in case they need to stay late.
If your job is more flexible, this problem may be hard to relate to. But open discussions can help both of you know what to expect and plan accordingly.
5. A Vet’s Job is Physically Demanding
Animal patients may be nervous, energetic, aggressive, or wiggly. They don’t hold still for their examinations the way human patients do.
Your partner probably spends a large portion of the day crawling on their hands and knees to palpate a dog on the floor, hunching over to get a better look at a skin mass, or even lifting and restraining a patient on the x-ray table if extra hands are needed for the task.
Plus, vets are on their feet all day.
So, don’t be surprised if your partner comes home and collapses onto the couch. Helping them with the little things (like laundry and cooking) can go a long way toward letting them recharge.
6. Veterinarians Are Used to Talking about Gross Stuff
Gross stuff—such as anal glands or draining pus from an abscess—are a normal part of the day for vets. As such, it’s something they’ve grown very comfortable seeing and talking about.
If your partner brings these things up at dinner and makes you gag while you’re eating, they’re not trying to be insensitive.
They’re just so acclimated to these things that they might not realize how it affects others to hear about them. A polite reminder is all that’s needed if it bothers you.
7. Lots of People Ask Veterinarians Questions Outside of Work
In addition to being introverted, there’s one more big reason why vets might want to avoid social situations…
That is, they often don’t get to enjoy themselves because people ask them all sorts of questions about their pets, or tell them sad stories (such as the time they had their pet euthanized), once they find out that person is a vet.
While veterinarians can be passionate about what they do, they still need a break sometimes. It’s not healthy for anyone to take their work home with them to this extent.
You can help your spouse by establishing boundaries with well-meaning friends and family members, being understanding if your partner doesn’t feel like going out, or at least rescuing them if you see someone’s got them cornered at a party.
8. Many Vets Graduate with Significant Student Loan Debt
Since finances are the most common cause of divorce, it’s important to confront all financial issues head-on—and student loans are a part of that.
Being open and honest with each other, exploring options for repayment, and talking to a qualified financial professional can all help make student loans more manageable and less stressful.
These steps will help you feel like a team as you tackle your financial future.
Supporting Each Other
While veterinary medicine carries its own unique stressors, it’s important for YOU to feel supported in your job and relationship, too.
Open and compassionate communication can help both of you establish what you need from each other and maintain a healthy, happy relationship. Talking to a counselor or other professional can also help with big issues or stressful times.
Having each other’s backs will ensure you work together toward your goals and have a lot of fun along the way.
Written by: Dr. Tammy Powell, DVM
Retirement Plans for Veterinarians: Key Considerations
Retirement from veterinary medicine is a big step—a break that many look forward to after years of hard work, but also something that can cause boredom or confusion as to what comes next.
If you’re nearing retirement as a veterinarian, no matter what your age, here are some things to consider…
When Can You Afford to Retire?
Retirement planning is still a mystery to many people. To say the least, it’s a complex subject.
For example, social security or other benefits vary depending on which age you retire. And there are harsh tax penalties for dipping into retirement savings too early. Do you plan to sell your practice before you retire?
Also, expenses often go up during retirement—which means a person may need more money than they expect.
Some of this is due to increasing medical needs that naturally occur with age. Some is due to pursuing new interests—such as classes, hobbies, travel, or entertainment—more often now that work obligations don’t get in the way.
For all these reasons, it’s a good idea to consult with a financial advisor you trust. The process and planning often start years in advance.
Financial professionals can help you crunch the numbers, make sure there’s nothing you’re forgetting, and help you truly feel secure about when is the best time for you to retire.
What Does Retirement Look Like to You?
Retirement could mean giving up veterinary work entirely. Or, it could mean working 1-2 days a week, working in a different capacity (for example, teaching at a vet tech school rather than being in clinical practice), or anything in between.
This decision is a personal one. Sometimes, a person will transition to retirement slowly due to financial reasons or simply because they still enjoy their work.
What Will You Do Next?
Whether or not you continue part-time veterinary work, you will probably find yourself wanting to pursue other interests now that you have more time.
It’s natural for a person who’s worked hard for years to spend time relaxing when they retire. But eventually, most people would want to devote their time to things that spark their curiosity and passion.
This could mean veterinary work in a new capacity, such as volunteering internationally or becoming a consultant for veterinary practices, or perhaps training dogs or owning and riding horses.
Or, it could mean starting something new that has nothing to do with veterinary medicine.
Many veterinarians view their career as part of their identity, so it may feel strange to move on to something new during retirement. However, you’ll always be a veterinarian, even if you aren’t practicing. You’re also a multi-dimensional person, so it’s okay to explore those other aspects of yourself now that you have more time.
For example, maybe you’d like to write a book, volunteer for non-profits, start a community garden, start a band, go back to school for a new career, or pursue some other passion.
So long as you’re responsible with your finances, there’s really no limit. You’ve worked hard, so you deserve to find something that lights you up!
Should You Keep Your Veterinary License in Retirement?
There’s truly no right or wrong answer. The best solution will vary from person to person.
Many vets do prefer to keep their license as “insurance,” in case they’d like to go back into practice for any reason—such as missing their work or needing a little extra income. And some states allow a vet to place their license on “inactive” status, which may be easier to maintain.
Maintaining a license makes sense, considering it’s usually much easier to keep up a license than to reinstate one that’s lapsed. But a retiring veterinarian should consider what will work best for them.
The same is true of malpractice insurance (some types cover incidents that happened when the policy was in place, even after the policy is canceled, while others only provide coverage while the policy is active) or other factors that may be relevant.
Make Your Retirement What You Want It to Be
By considering the many possible factors that could affect your retirement—including financial, legal, family considerations, boredom and finding a new direction, and anything else that may affect you and your loved ones—you can plan this next step of your life to be a satisfying change.
You may still change your mind about what to do during retirement as time goes on. But planning ahead will help ensure you have the most options—and that your retirement can be as smooth and meaningful as possible.
Written by: Dr. Tammy Powell, DVM
Selling Your First Practice as a Veterinarian
Table of Contents
As a veterinarian, the decision to sell your practice can mean a mix of emotions and a very long to-do list, but it can also result in satisfaction and cash flow with which to start your next venture in life.
Starting your first veterinary practice is no easy feat. You put a lot of time and energy into it, whether you bought into an existing business or built it from the ground up. And you poured yourself into gaining clients and patients.
When it comes time to sell, it makes sense to put in due diligence to ensure you’re getting a fair price after all the work you put into growing the business. Here are a few things to consider…
The Decision to Sell
Maybe you’re ready to retire. Maybe you’re ready for a change in career path, such as going back to school for a specialty, starting a larger hospital, or trying a new career altogether.
Maybe your spouse got a job out of state, or you want to spend more time at home with your children. Or maybe you’d just like a break from all the responsibilities of owning a business.
Whatever the reason, you’ve decided that it’s time to sell your first practice. This isn’t necessarily an easy decision, especially since your first practice represents a lot of hard work and many special memories.
So, it’s only natural to take your time.
Mull it over.
Build lists of pros and cons and goals for the sale.
And discuss it with non-work friends and family that you trust.
Creating a Gameplan
Once you make the decision to sell, the next step is to create a plan.
The first decision is probably when to sell. Of course, this isn’t entirely within your control, as it will depend on when you find a buyer.
But to start, do you want to sell right now?
Or, are you planning ahead for five years from now—and investing to grow the practice’s value in the meantime?
Are you hoping to stay on at the practice a few more years, even if it’s just part-time? Or are you planning to exit after the sale?
If you had your preference, who would you sell to?
Maybe there’s an associate at your practice who’s interested in ownership and could work up to it over the next few years by buying in gradually. And maybe you have a strong preference for a private buyer versus a corporate buyer.
While there may be some need for flexibility depending on the offers received, it’s good to have goals in mind to help steer your decisions.
Also, how much money would you like to make in the sale? This is probably the hardest question. In addition to the need to carefully consider personal, ongoing financial requirements, many practice owners find it difficult to guess what their practice could actually sell for.
That’s not surprising, considering that the calculations are very complex. The old way of thinking (i.e., one year’s gross income) is often not accurate.
Fortunately, there are many professionals who can help with these specialized aspects of the sale.
Gathering Your Team
As with any other professional venture that requires expertise, it’s good to consult specialists in each area of the sale. This could include…
A practice/valuation consultant.
A CPA.
Attorneys (for business, real estate, etc.).
A broker (if needed—in general, they are of the most value when finding a buyer is challenging).
Any other experts that could be helpful.
These professionals can help with a myriad of issues—everything from minimizing taxes paid on the sale, to advising on provisions such as a non-compete clause for current employees (something that can affect the perceived value of the practice).
Be sure to ask about their charges, but don’t be scared to pay a reasonable rate.
As tempting as it is to save money and try to do everything yourself, these experts can really save a lot of headaches and prevent costly mistakes.
Many vets prefer professionals who charge a flat fee rather than a percentage of the sale, but this depends on your inclination and the specifics of your sale.
Taking Care of Your Staff and Clients
Many experts advise not talking to your staff about the sale until the paperwork is finalized. The worry is that, although a sale may take years, team members may grow worried and begin to look for another job.
However, when the time comes, it’s a good idea to spend time discussing what they can expect. Inform them of your confidence in the new owner, and answer questions if you can (although don’t guarantee anything such as job security unless you know for sure).
So far as your patients and clients, you have probably grown close to many of them.
A letter or email sent to current clients, informing them of the change and your confidence that they will love the new doctor/management, can do a lot to help them during the transition, as well as set up the new practice owner for success. Some clients may also wish to say goodbye before you leave.
What’s Next?
It can be normal to have a period of feeling lost or even grieving, after the sale of a practice.
After all, it’s a big change.
You’re probably excited for whatever comes next. Or, if you haven’t found your next venture yet, spend some time exploring your curiosities and interests.
Do things that light you up, and eventually, you’ll figure out what’s next for you.
While selling a practice is no easy feat—just like starting a practice wasn’t easy—it can also be a rewarding experience.
Hopefully, the sale will help fund whatever is next for you in life, whether that’s a new professional venture or a more relaxed pace in life.
Either way, you can always look back with satisfaction on what you created, and all the pets you helped along the way.
Written by: Dr. Tammy Powell, DVM
Adjusting to Life as a New Veterinary Graduate
Table of Contents
The time after graduation can be an exciting period of learning, making new connections with colleagues and clients, and figuring out what you’d like your career to look like. However, even though veterinary school provides a wonderful education, sometimes the transition to the “real world” of clinical practice can feel challenging.
Here are some things to consider to make this transition smooth and enjoyable…
Going from School to Clinical Practice
In many ways, school and clinical practice are similar. After all, school focused on the knowledge and skills someone would need to be a practicing veterinarian.
However, new grads and experienced vets alike have pointed out some key differences.
For example, even with a thorough education, many vets don’t see every possible type of medical case in school—so they might see their first GDV or unblock a urinary obstruction in a cat by themselves for the first time in clinical practice.
While new vets have the tools and knowledge to handle all of these situations, some may find that it feels a little intimidating to be in charge of these cases for the first time.
Learning how to talk to clients can also take experience and practice—especially when it comes to discussing costs.
Unlike at a university teaching hospital, where many pet owners could afford treatment with a specialist, clients in many locations of the country simply can’t afford to do as much as they would like to do for their pets.
Therefore, vets must often gain the skill of discussing why everything in “Plan A” is recommended, what are the risks of not doing all recommended diagnostics and treatments, and then discussing alternative treatment plans (when possible and reasonable for the pet’s comfort and safety).
All of this may seem kind of overwhelming in a vet’s first job.
Fortunately, there are resources to help.
Learning and Finding the Resources You Need
Mentorship is valuable for anyone entering a new profession—and veterinarians are no exception.
A mentor could be another person (or multiple people) who works at your practice. This often includes other vets who are open to mentoring (or at least having a collaborative workplace), since they have been through this transition themselves after their own graduation.
But other support staff, especially experienced technicians or nurses, can also give valuable input and advice.
Mentorship can also mean keeping in touch with classmates, teachers, and former colleagues, or joining an online community such as VIN.
Conferences—both large gatherings and smaller or local events—and continuing education courses are also valuable, and many are available online nowadays.
Figuring Out Who You Want to Be as a Veterinarian
While mentorship is very valuable, there will come a time when you develop your own style of practicing medicine. You and your colleagues may have differing opinions on some things—and so long as you are providing great care to your patients, that’s okay, because even specialists don’t agree on everything.
Your own practice style could include your professional interests. For example, you could become the “go-to” doctor at your practice for dentistry, nutrition, or exotics, or you may decide you want to go back for a residency in your preferred specialization.
Your practice style will also include deciding what you are (or aren’t) comfortable doing as a vet, such as declaw surgeries.
Finding Work-Life Balance
Since burnout and stress are common in the profession, it’s best to set up healthy habits—such as meditation, getting enough sleep, socializing, pursuing hobbies, etc.—from the beginning. If these habits seem daunting, start small at first. For example, spend 10-15 minutes on a hobby or meditate for 5 minutes if that’s all you can spare.
If stress arises at the new job, asking for help (from a friend or professional therapist) can make a world of difference.
There are even some veterinary-specific organizations that are there to help, such as
A Few More Tips
Remember to prepare for student loan payments, if that applies to you.
They typically kick in six months after graduation.
Use a budgeting system, or speak to a financial professional, to ensure your hard-earned salary is used wisely to provide the lifestyle and secure future that you want.
And remember, they call it the “practice” of medicine for a reason.
There is always some degree of learning that happens on the job, and even experienced practitioners can see new things that surprise them.
So, it’s important to give yourself grace if you feel like you don’t know everything.
Just remember your list of resources and mentors when you need a second opinion on a case.
Know that it will probably take you longer than a more seasoned colleague to research a new case, create a treatment plan, and write up the medical record.
But, you’ll get faster with time and practice, and you’ll eventually find a routine that works for you.
Though the first job after graduation from vet school can feel intimidating, it can also be exciting and fun.
Preparation, along with an openness to learning new things along the way, can really set up a new grad for success in veterinary medicine.
Written by: Dr. Tammy Powell, DVM
Creating a Support System for Veterinarian Families
Balancing Parenthood & Veterinary Careers: Key Strategies
It can be challenging to balance the roles of “veterinarian” and “parent”—but fortunately, many veterinary professionals find ways to make it work. It helps to have strategies for planning ahead and finding a support system.
Childcare Solutions for Veterinary Professionals
Balancing parenthood and a career in veterinary medicine can definitely present challenges. One of the biggest aspects to consider is time and flexibility. Clinical practice can carry long hours. Often, these hours aren’t flexible, especially when the appointment schedule is packed or when patients need urgent or emergency care.
All of this can make it difficult to leave to pick a child up from school, stay home to care for a sick child, or make it to a child’s soccer game—to name a few examples.
A busy and tired vet professional might also feel discouraged if they seem to be missing out on quality time with their child.
Additionally, there are cost considerations, since raising a child can be expensive! This becomes even more of a factor should a child have special needs.
While there are other considerations when it comes to being a veterinary professional and having children, these are some of the biggest and most frequently cited concerns. Add to this the fact that the veterinary profession is predominantly female in recent years—and (for better or for worse), in our society, many childcare and home care duties often still fall to females, even if they are employed—and it’s easy to see that veterinarians can benefit from strategies for balancing career and family.
Veterinary Work-Life Balance: Childcare Tips & Ideas
There’s an old saying that “It takes a village to raise a child.” However, in modern society, it seems we’re often expected to “do it all.” We’re busier than ever. Since the pandemic started, many of us have had to handle life’s responsibilities while feeling isolated, too.
Is there a way to get back to that “village” mentality? Many experts argue that developing close relationships with extended family and friends is healthy for a child, even at a very young age. And a child’s parents may benefit from having a healthy network of mutual support.
Here are a few ideas for where and how help can be implemented…
Spouse or partner. If a parent is in a relationship, it’s important to discuss the sharing of responsibilities. This is not just for childcare, but also for household duties like cooking, cleaning, doing the budget, and more. Having a partner take on some of these tasks can give the vet professional more time to spend with their children.
Hiring help. If it’s at all reasonable for the budget, it may make sense to hire someone to help—like a nanny, babysitter, or someone to pick up or drive the kids when needed.
Additionally, it may help to hire someone to clean the home, to send out laundry, or to use a meal delivery service. Nowadays, many services can be scheduled via apps. These service providers free up valuable time and energy for the vet professional. In addition to making it a bit easier to parent, this freeing up of time may also help with physical and emotional health.
Extended family. Maybe the children’s grandparents or aunt/uncle live nearby and would love to spend some time with the kids. While being respectful of their time and obligations, it may be worth it to check with these family members about taking the kids after school until you get home from work.
Friends. Maybe you have close friends or neighbors who wouldn’t mind helping from time to time—especially if they have children of their own and you could return the favor at another time.
Of course, not all of these options will be available to everyone. But, brainstorming all possible options, and planning ahead, gives the best chance of having support when it’s really needed.
Making Arrangements at Work
If you’re struggling with finding childcare, consider the best way to talk to your employer about how this could affect your work. They may surprise you by being open to making allowances—such as allowing you to pick up your children from school and then return to work.
If you must leave work early for an emergency or for an event such as a child’s dance recital, your coworkers may be able to fill in and help, too.
However, in all of these scenarios, it’s important to be courteous to the needs of colleagues, too. Everyone has their own obligations in life. Many people may have things that take up time and emotional energy—such as a chronic illness, a parent with dementia, a battle with depression, etc.—that they don’t talk about at work.
So, don’t assume it will always be easy for child-free coworkers to cover the time you miss, or to see your patients if you must leave suddenly. Instead, try to arrange a swap. Or, offer to make up the time in the case of an emergency. Also, children should be well-behaved if they are brought to the workplace. That way, everyone feels mutually respected, and the workplace can be supportive of everyone’s needs over the long term.
Pre-Parenthood and Maternity Leave
If you’re in a position where you’re planning to have a family in the next couple of years, it may be beneficial to plan ahead and take a serious look at your current (or prospective) job and how that fits into your plan.
For example, are there others working there who have children—and how are they managing it? How flexible and conducive to parenting needs is the workplace?
Also, what are the benefits like? Is there paid maternity (or even paternity) leave? In cases of small practices that might not be able to afford extended maternity leave, does it seem like they are still trying their best to accommodate employees who have recently become parents?
Would a career shift (to industry, academia, or relief veterinary services, for example) be a better fit for you at this time?
Another consideration would be for vet professionals who are considering fertility treatments or need other medical care to become a parent. Could the workplace accommodate the many appointments that would be needed during this time?
Being a Pet Parent
Many veterinarians and team members view their pets as children—regardless of whether or not they also have two-legged kids.
So, it may also be worth it to look into factors such as whether or not you can bring your dog to work so they’re not home alone all day, and what sort of discount is available to employee pets.
Conclusion
Families come in all shapes and sizes. Every family will have unique needs, and balancing work and family may be difficult at times.
However, by finding the best possible work arrangement for their situation and creating a “village” of support, many vet professionals make parenthood work for them!
Written by: Dr. Tammy Powell, DVM